MEMO
TO: Senator Patty Murray, Ranking Member, Senate Health, Education, Labor and Pensions Committee
FROM: Jennifer J. Frost, DrPH, Principal Research Scientist, Guttmacher Institute
Mia R. Zolna, MPH, Senior Research Associate, Guttmacher Institute
DATE: May 3, 2017
SUBJECT: Response to Inquiry Concerning the Availability of Publicly Funded Contraceptive Care to U.S. Women
We are writing in response to your inquiry for updated data on the availability of contraceptive care from safety-net family planning centers in the United States, particularly the role of Planned Parenthood in meeting women’s need for publicly funded contraceptive care. We are also responding to your request for information on how readily community health centers—here referred to as federally qualified health center (FQHC) sites—would be able to serve all of the women currently obtaining contraceptive care from Planned Parenthood health centers and other safety-net providers currently supported by the Title X national family planning program.
In order to respond, we have updated and expanded on an analysis that we conducted at the request of the Congressional Budget Office in 2015 (using 2010 data).1 Unless otherwise noted, the information presented in this analysis comes from 2015 data published in a recent Guttmacher report2 or special tabulations of those data. These data were obtained through a comprehensive census of the more than 10,000 safety-net health centers that provide contraceptive care in the 50 states and District of Columbia. Data were obtained on the location and numbers of female contraceptive clients served at all sites according to the type of center providing care (FQHC, health department, hospital, Planned Parenthood or other independent site). Tables detailing these new tabulations are attached; key findings are highlighted in the text and in a series of graphics.
How many FQHCs currently provide contraceptive care?
Not all FQHC sites provide contraceptive care.
- In 2015, FQHCs operated 9,636 services sites in the 50 states and the District of Columbia.3 Of these, 5,829 (60%) reported offering contraceptive care to at least 10 female clients; as such, they are considered safety-net family planning centers (see Key Definitions).
What would be the impact of "defunding" Planned Parenthood?
Planned Parenthood health centers serve a considerable proportion of all safety-net contraceptive clients (see Key Definitions).
- Nationally, two million (32%) of the 6.2 million contraceptive clients served by safety-net family planning centers are served at Planned Parenthood health centers (see Table 1).
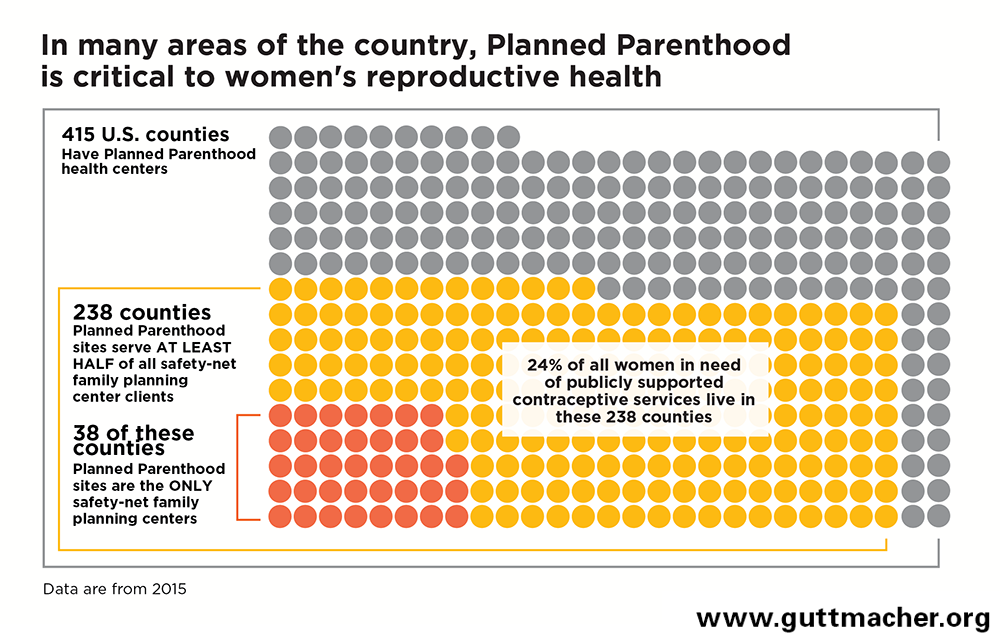
Planned Parenthood sites are a critical source of care in the communities where they are located (see chart below).
- Planned Parenthood health centers are located in 415 U.S. counties (see Table 2).
- In 238 (57%) of the 415 counties with a Planned Parenthood health center, Planned Parenthood serves at least half of all safety-net contraceptive clients (see Table 2).
- In 38 of these counties, Planned Parenthood serves all safety-net contraceptive clients (see Table 2).
Two-thirds of all U.S. women in need of publicly funded contraceptive care live in counties where Planned Parenthood health centers are located (see Key Definitions).
- Nationwide, 20.2 million women are in need of publicly funded contraceptive care (see Table 2).
- Sixty-four percent (12.9 million) of these 20.2 million women in need of publicly funded contraceptive care live in the 415 counties with a Planned Parenthood health center (see Table 2).
- Twenty-four percent (4.8 million) of women in need of publicly funded contraceptive care live in the 238 counties where Planned Parenthood serves the majority of women who obtain contraceptive care at a safety-net family planning center (see Table 2).
On average, Planned Parenthood health centers serve many more female contraceptive clients per year than do other types of safety-net family planning centers (see Key Definitions).
- Planned Parenthood health centers each serve an average of 2,950 female contraceptive clients per year.
- By contrast, FQHC sites each serve 320 female contraceptive clients on average per year; health department sites serve 560, centers operated by hospitals serve 720 and centers operated by other types of agencies serve 460.
Overall, Planned Parenthood health centers serve a greater share of safety-net contraceptive clients than do any other type of provider.
- Although Planned Parenthood health centers represent only 6% of all safety-net family planning centers, they serve 32% of all safety-net contraceptive clients.
- Sites operated by FQHCs serve 30% of safety-net contraceptive clients, health department sites serve 20%, centers operated by hospitals serve 10%, and centers operated by other types of agencies serve 8%.
If legislation that "defunds" Planned Parenthood became law, how readily could FQHCs provide the contraceptive care now provided by Planned Parenthood?
FQHC sites providing contraceptive care would have to considerably increase their client caseloads in order to serve all the female contraceptive clients currently served by Planned Parenthood (see Key Definitions).
- Nationwide, the network of FQHC sites provide contraceptive care to 1.9 million women a year (see Table 1).
- To serve all the contraceptive clients currently served by Planned Parenthood health centers, FQHC sites would have to double their safety-net contraceptive client caseloads, to 3.9 million contraceptive clients (see Table 5).
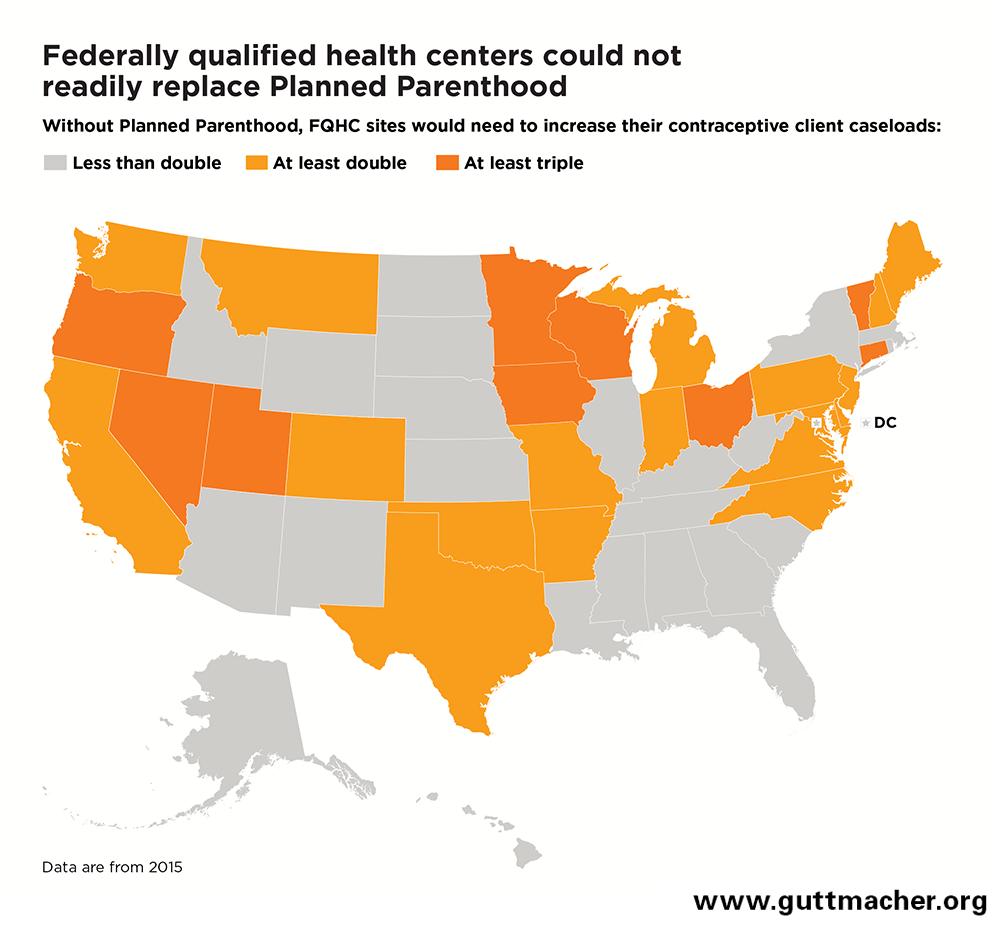
FQHC sites providing contraceptive care in all but one state (North Dakota, which lacks any Planned Parenthood centers) would have to expand their capacity in order to serve all of the safety-net contraceptive clients served by Planned Parenthood (see map below).
- In 27 states, FQHC sites would have to at least double their contraceptive client loads (see Table 1).
- In nine of these 27 states, FQHC sites would have to at least triple their contraceptive client loads.
- In about half of states, FQHC sites would have to expand to accommodate tens of thousands of additional clients now served by Planned Parenthood health centers (see Table 1).
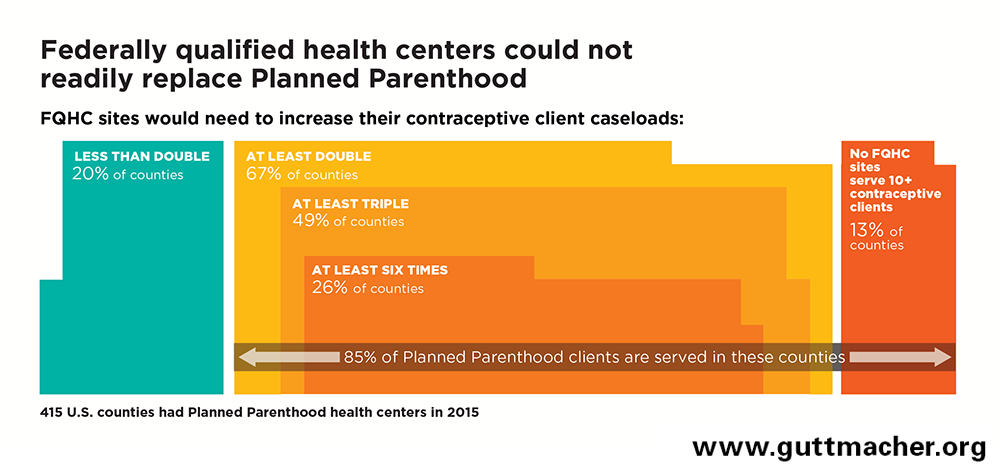
In the 415 counties with Planned Parenthood health centers, FQHC sites providing contraceptive care would have to substantially expand their capacity in order to serve all of the female contraceptive clients currently served by Planned Parenthood (see chart below).
- In 54 (13%) counties with Planned Parenthood health centers, there are no FQHC sites offering contraceptive care; 4% of Planned Parenthood’s female contraceptive clients live in these counties (see Table 3).
- In 38 of these 54 counties, there is no other safety-net family planning center of any kind (see Table 2).
- In 279 (67%) counties with Planned Parenthood health centers, FQHC sites providing contraceptive care would have to at least double their capacity; 81% of Planned Parenthood’s female contraceptive clients live in these counties (see Table 3). In most of these counties, FQHC expansions would have to be much more substantial:
- In 203 of these 279 counties, FQHC sites would have to at least triple their existing contraceptive client caseloads; 49% of Planned Parenthood’s female contraceptive clients live in these counties.
- In 108 of these 279 counties, FQHC sites would have to increase their existing contraceptive client caseloads by a factor of at least six; 22% of Planned Parenthood’s female contraceptive clients live in these counties.
- In only 82 (20%) counties with Planned Parenthood health centers, FQHC sites would have to increase their capacity by less than double; 15% of Planned Parenthood’s female contraceptive clients live in these counties (see Table 3).
- Of all Planned Parenthood’s contraceptive clients, 1.7 million (85%) live in the 333 counties where FQHC sites would have to at least double their capacity, or where there are no FQHC sites providing contraceptive care (see Table 3).
Compared with FQHC sites that offer contraceptive care, Planned Parenthood health centers do more to facilitate women’s timely access to high-quality contraceptive care.4,5
- Nearly all (93%) Planned Parenthood health centers offer the full range of contraceptive method options, while 52% of FQHC sites do so.
- While 83% of Planned Parenthood health centers offer oral contraceptive supplies and refills on-site, 34% of FQHC sites do so.
-
More than three-quarters (81%) of Planned Parenthood health centers offer insertion of IUDs and implants on the same day as a client’s initial appointment, while 25% of FQHC sites do so.
How readily could FQHCs become the sole providers of contraceptive care currently supported by the Title X program?
The Title X national family planning program supports 3,700 safety-net family planning centers operated by a range of agency types throughout all 50 states and the District of Columbia (see Table 1).
- There are Title X–supported sites in 2,015 (64%) of the 3,142 U.S. counties (see Table 1).
- Of all sites that receive Title X funding, 13% are operated by Planned Parenthood affiliates, 26% by FQHCs, 48% by health departments, 4% by hospitals and 9% by other types of agencies.
Where there are both FQHC sites providing contraceptive care and Title X–supported providers that are not FQHCs, the FQHCs would have to substantially increase their female contraceptive client caseloads in order to serve all those who now obtain Title X–supported services.
- Nationwide, FQHC sites providing contraceptive care would have to increase their contraceptive client caseloads more than two and a half times over current service levels, to five million clients (see Table 5).
FQHC sites providing contraceptive care in every state would have to increase their capacity in order to serve all of the female contraceptive clients currently served at non-FQHC Title X sites.
- In 41 states, FQHC sites would have to at least double their female contraceptive client caseloads (see Table 1).
- In 27 of these 41 states, FQHC sites would have to expand even more, at least tripling their female contraceptive client caseloads.
- The District of Columbia is the only place where FQHC sites are the sole Title X–supported providers (see Table 4).
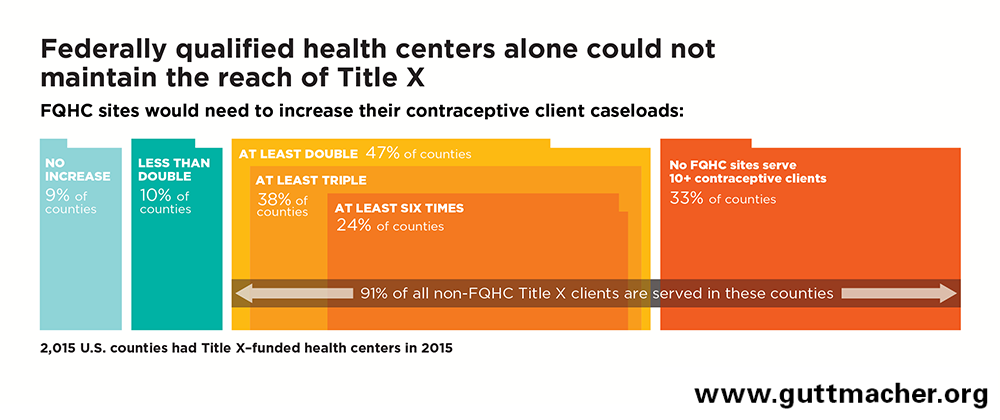
Among the 2,015 counties that have a Title X–supported site, most FQHC sites offering contraceptive care would have to substantially expand their capacity in order to serve all of the female contraceptive clients currently served by non-FQHC Title X centers (see chart).
-
In 670 (33%) counties with a Title X site, there is no FQHC site that provides contraceptive care; 11% of contraceptive clients served at non-FQHC Title X sites live in these counties (see Table 4).
-
In 955 (47%) counties with a Title X site, FQHC sites would have to at least double their existing contraceptive client caseloads; 80% of safety-net contraceptive clients served at non-FQHC Title X sites live in these counties (see Table 4). In most of these counties, FQHC expansions would have to be much more substantial:
-
In 774 of these 955 counties, FQHC sites would have to at least triple their existing contraceptive client caseloads; 53% of safety-net contraceptive clients served at non-FQHC Title X sites live in these counties.
-
In 493 of these 955 counties, FQHC sites would have increase their existing contraceptive client caseloads by a factor of at least six; 30% of safety-net contraceptive clients served at non-FQHC Title X sites live in these counties.
-
-
In 390 (19%) counties with Title X sites, FQHC sites are either the only Title X provider (183 counties) or would have to increase their capacity by less than double (207 counties); 9% of safety-net contraceptive clients served at non-FQHC Title X sites live in these counties (see Table 4).
-
Of all contraceptive clients served at non-FQHC Title X sites, 2.8 million (91%) live in the 1,625 counties where FQHC sites would have to at least double their capacity, or where there is no FQHC site providing contraceptive care (see Table 4).
Key Definitions
Safety-net family planning center: A health center that offers contraceptive care to the general public and uses public funds (e.g., federal, state or local funding though programs such as Title X, Medicaid or the federally qualified health center program) to provide free or reduced-fee services to at least some clients. Sites must serve at least 10 contraceptive clients per year. These sites are operated by a diverse range of provider agencies, including public health departments, Planned Parenthood affiliates, hospitals, federally qualified health centers and other independent organizations.
Federally qualified health center (FQHC): Federally qualified health centers (often referred to as community health centers) are community-based health care providers that receive federal funding under Section 330 of the Public Health Services Act to provide primary care services in underserved areas. FQHCs must offer comprehensive preventive and primary care services (including family planning services) either directly or through contracts or cooperative agreements with other agencies. One FQHC may operate a number of individual service sites. For purposes of our analysis, so-called FQHC "look-alikes" (organizations that meet eligibility for Section 330 support but do not receive grant funding) are not included in this category.
Title X–supported center: A site that receives federal funding through the Title X national family planning program.
Female contraceptive client: A woman who made at least one initial or subsequent visit for contraceptive care during the 12-month reporting period covered by this data collection effort. This includes all women who received a medical examination related to the provision of a contraceptive method, made supply-related return visits, received contraceptive counseling and a method prescription but deferred the medical examination, or chose nonmedical contraceptive methods, even if a medical examination was not performed, as long as a chart was maintained.
Safety-net contraceptive client: A female contraceptive client who obtained that care from some type of safety-net family planning center, rather than a private physician.
Women in need of publicly funded contraceptive care: Those women who a) are younger than 20 or are poor or low-income (i.e., have a family income less than 250% of the federal poverty level) and b) are sexually active and able to become pregnant but do not want to become pregnant.
Increasing female contraceptive client caseloads: An estimate of the factor or percentage by which FQHC sites providing contraceptive care would have to increase their provision of services to female contraceptive clients if they: a) had to serve all such clients currently served by Planned Parenthood health centers or b) had to serve all those currently served by other types of Title X–supported centers. These estimates reference Tables 3, 4 and 5. For example:
- If other sites serve 100–199% of the number of current clients as do FQHC sites, then FQHC sites would have to at least double their existing client loads in order to serve their own female contraceptive clients and those currently served by other safety-net family planning centers.
- If other sites serve 200–299% more clients (at least twice as many) as do FQHC sites, then FQHC sites would have to at least triple their existing female contraceptive client loads.
- If other sites serve 300–399% more clients (at least three times as many) as do FQHC sites, then FQHC sites would have to at least quadruple their existing female contraceptive client loads.
- If other sites serve 400–499% more clients (at least four times as many) as do FQHC sites, then FQHC sites would have to increase their existing female contraceptive client loads at least by a factor of five.
- If other sites serve 500–599% more clients (at least five times as many) as do FQHC sites, then FQHC sites would have to increase their existing female contraceptive client loads at least by a factor of six.